Avkin: How Far We’ve Come

I never saw myself as a CEO of a company. Yet here we are. Avkin entered its sixth year, released its eighth wearable device, and offers an entire educational services suite. I have an incredible and passionate team working alongside me each day toward our shared dream. So, while we’ve come far, I would be lying to say we’ve fully arrived.
However, it’s always good to look back at our humble beginnings and celebrate just how far we’ve come.
A Lesson in Fidelity
I was working in an emergency room when I found a job posting for the University of Delaware School of Nursing. I was intrigued by the clinical skills and simulation lab position and had wanted to give back to the next generation of nurses.
When I started, I was handed two large manikins with instruction to integrate them into the curriculum. After a quick online search, I developed a cursory understanding of what I was supposed to do. I also quickly realized that my students truly struggled to communicate with the manikin, a problem that interfered with accomplishing learning objectives.
Armed with my giant, lifeless, plastic people, I decided a code blue scenario would be an ideal simulation. It seemed perfect; no communication was required with the manikin. All the students needed to do was perform CPR. This would turn out to be my first true lesson in simulation fidelity.
During one of our simulations that day, our learner came in, and the simulation was moving as expected. She was performing chest compressions when I called the code overhead to begin postmortem care. However, once the student heard the date and time of expiration, she took her hands, smacked them into the chest of the manikin, and says “That’s it. You’re dead. I am done.”
Thankfully, the look of horror on my face was hidden by the one-way glass, but I could not escape the thought that this manikin represented a human being. This was someone’s father or brother, and here my student was abusing a corpse. It was quickly apparent that my students were not associating the manikins with human life; Was I teaching my students to take care of plastic and not people?
People, not Plastic
I needed living people involved in my simulation. I tried to contact the theater department on campus over several semesters but never could get a response. But, I was forced to put this on the back burner, where it stayed for some time.
Interprofessional simulation was the newest topic in the simulation world, and I sought to conduct one such simulation. In the planning phase, I showed the Physical Therapy educators my manikins, but they quickly dismissed the ability to use them. Instead, their learners needed to get patients out of bed and examine muscle tone. As an alternative, I offered my idea of using theater students, and I got lucky. They had a contact they said would be perfect.
I met with Allan Carlsen with the University’s theater department. I fully expected him to just send me a few volunteers. Instead, we wound up starting an independent study for four of his students!
That spring, we conducted our first interprofessional simulation between nursing and physical therapy, with theater students as the patients. The evaluations were through the roof; the students loved the opportunity to work with live people. Walking in the parking lot later that day with Allan, he said, “this is going to be a boiling pot you have trouble keeping the lid on.”
At the time, I couldn’t see what this program would turn into. But then we began to expand with psych, diversity, and interprofessional simulations, all happening with theater students enrolled in a college course. My learners were much better served by this arrangement, and even the theater students were honing their skills. I was delighted in my own little world.
An “Aha!” moment
Unfortunately, I was recalled to work with the manikins after my replacement abruptly left. While I was disappointed, this opportunity was the perfect example of the difference between simulations with manikins and simulations with people.
One of the last simulations for the semester was a tracheostomy simulation. The students were expected to come in, evaluate, and then suction the patient, Mr. Jones.
This particular group entered the room, and after introducing themselves, asked for Mr. Jones’s name. As you’re aware, tracheostomy patients are non-verbal on account of a device in their trachea, so I remained silent. The students looked at the quiet, lifeless manikin and declare, “Oh my goodness. He is dead!” In their haste, they caused an occlusion which eventually led to chest compressions.
A far cry from suctioning the trach, I sat back in the control room wondering how we got here and whether there was some way to get a theater student to wear the trach.
Inspired by my success working with the theater department, I started to reach out to the school’s engineering department. I was quickly connected with Jenny Buckley, who conducted a senior-level course where engineering students had 15 weeks to take a project from concept to prototype. At first, there were some objections, namely, “electronics and fluids do not mix in products.” However, because they were in a course, I was able to tell them that they had 15 weeks to figure it out.
And figure it out, they did. I was excited to receive my prototype that looked like it was held together with glue and gum (I say this in the most loving way possible.) When I finally put it on my theater student and had my nursing student suction, I had my Walt Disney moment. What was in my head was happening in front of me.
Taking it to the Masses
I started inviting simulation companies to visit the University to see our product. I honestly thought there would be a bidding war for this revolutionary step forward, but it did not happen that way. No one showed serious interest, so I signed up for a poster presentation at the International Meeting on Simulation in Healthcare (IMSH).
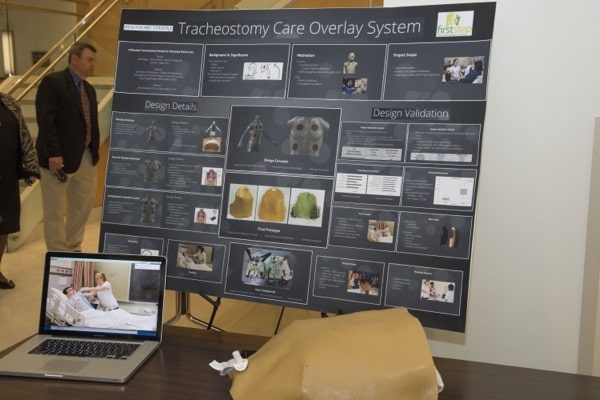
A few months later, we received an email telling us we won first prize. We won for Innovation and Technology.
It turns out we entered a contest.
And we won.
First prize.
A small team and I made our way to New Orleans to give a ten-minute presentation about what we had created. They began calling out the winners, and we waited patiently to be recognized. They called up third place: Yale. We beat Yale.
Second place was called for biomedical engineers from Harvard. WE BEAT HARVARD?!? It took everything in me to not jump for joy.
And finally, it was our turn. Our small but mighty team conducted our presentations to much acclamation. People were coming up to us, offering business cards and wanting to know when they could purchase one. ‘Now,’ I thought, ‘this is when we’ll get our bidding war.’
Well, then do it.
Later, on the exhibit floor, we talked with one of the simulation companies there. I showed them all of the business cards we received that day.
“I could have sold 50 of these out of the back of my van,” I told them.
“Well, then do it.”
At that moment, I knew if I didn’t drive this idea forward, it would never make it to the masses. I couldn’t wait for anyone else to adopt my dream. So I put on my CEO hat and started a company because I knew it was the right thing to do for the future of healthcare simulation.
Our small but mighty team persevered through the trials that come with starting a business and being a disrupter in a market. We found others who share our passion for preparing the next generation of healthcare providers. We’ve moved into our own building with in-house manufacturing to ensure quality, a Research and Development team dedicated to providing realism wherever possible, and a driven team serving educators worldwide.