A recent Nurse Blake TikTok poking fun at a nursing student calling SBAR to a provider made me think – why do we still struggle with communication? The answer: maybe because we don’t practice it. We practice skills and even complex scenarios, but when was the last time you debriefed on explicitly effective communication?
Hand off communications are fault lines for failures in patient safety (Müller, et al., 2018). While Nurse Blake’s parody illustrates the fear and uncertainty many of us came into healthcare with, it continues to be an area healthcare – all professions – fall short in. Yet, communication is paramount in leading us in realizing the vision of the Patient Safety Movement© Foundation to achieve ZERO preventable patient deaths by 2030.
Parallel to the shortcomings of aviation in the 1960-1970s, we continue with the insanity model here in healthcare. Truly, it can’t be because we don’t care. In my experience, never once has the answer to the question, “Why did you choose a profession in healthcare?” been anything other than the desire to help in some capacity.
Crew resource management, human factors and closed loop communication (CLC).
Why is it so resistive in healthcare? We’ve studied it, it’s been proven to work (Diaz, MD, FAAP, FACEP & Dawson, BSN, RN, CPEN, TCRN, EMT, 2020) (Hughes, et al., 2020), but here we are 21 years after the release of To Err is Human still contributing to the equivalent of crashing jumbo jets on a daily basis. Communication is key.
What are the blocks to implementing, adopting, buying in, and becoming experts at CLC if it is going to save lives? It works in other high stress fields such as the military and the nuclear industry, as well as some medical specialties that have followed the evidence (Baker, Day, & Salas, 2006).
The answer is simple.
We must train on communication.
We train on skills. We train on scenarios. How much emphasis or feedback are you providing to your learners on their communication skills. As the current state of technology encourages more and more non-verbal communication, this is a skill we must fight to include and emphasize in training rubrics and curriculum models. The good news, the research is already done and it is a critical component of training for many models used to train healthcare personnel such as TeamStepps® and American Heart Association® courses as well as many others. CLC defined by TeamSTEPPS®2.0:
Closed-loop communication is the process of acknowledging the receipt of information and clarifying with the sender of the communicated message that the information received is the same as the original, intended information. In essence, it is the process of confirming and cross-checking information for accuracy. This style of communication fosters the ability to ensure that the entire team has shared goals, expectations, awareness, and plan execution. (AHRQ, 2012)
Simply put, we must ensure our healthcare teams:
- Send a clear message;
- That message is heard as intended by way of a readback;
- and acknowledgement of order/communication completion.
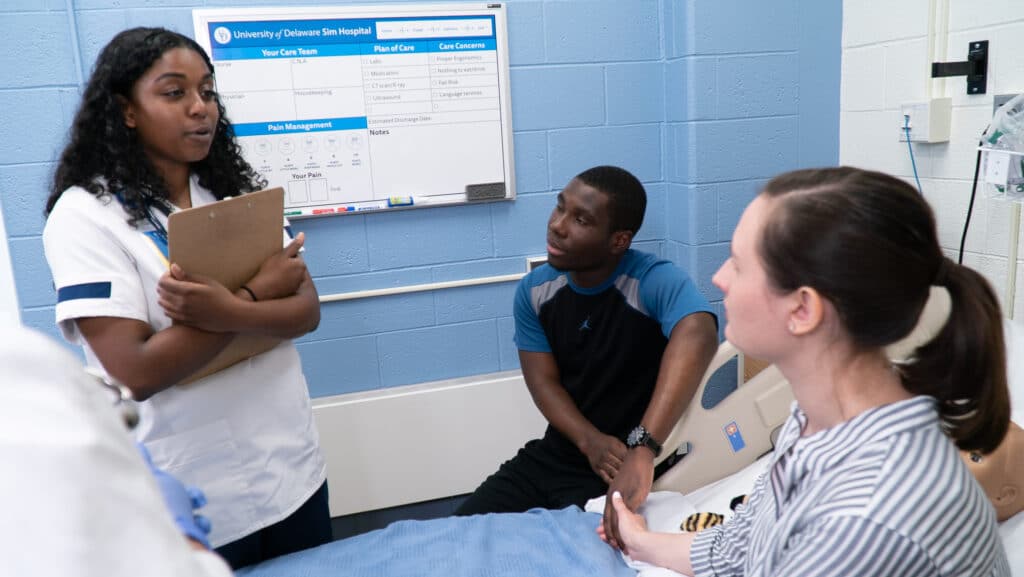
Not doing so leaves too much to chance and creates a seismic wave on that fault line to unsafe practice. Learners need time and training to effectively communicate. Communication training is going to be most realistic when providing learners the opportunity to work in teams and interacting with simulated participants (SPs). This most closely replicates their patient and staff interactions in the healthcare setting. To practice skills without incorporating communication is like learning a series of ballet moves and then going out on stage opening night to perform Swan Lake for the first time.
If you’re looking to integrate communications into your training, there are tools available to meet your needs. With both the Virtual SP Solution and Consulting Services, a tailor-made solution will be created to move your program into the 21st century.
References
AHRQ. (2012, September). TeamSTEPPS Fundamentals Course: Module 3. Evidence-Based: Communication. Retrieved May 8, 2021, from Agency for Healthcare Research and Quality: https://www.ahrq.gov/teamstepps/instructor/fundamentals/module3/ebcommunication.html
Baker, D. P., Day, R., & Salas, E. (2006). Teamwork as an essential component of high-reliability organizations. Health Services Research, 41(4 Pt 2), 1576-1598. doi:doi:10.1111/j.1475-6773.2006.00566.x
Diaz, MD, FAAP, FACEP, M. G., & Dawson, BSN, RN, CPEN, TCRN, EMT, K. (2020). Impact of Simulation-Based Closed-Loop Communication Training on Medical Errors in a Pediatric Emergency Department. American Journal of Medical Quality, 35(6), 474-478. doi:https://doi.org/10.1177/1062860620912480
Hughes, K. E., Hughes, P. G., Cahir, T., Plitt, J., Ng, V., Bedrick, E., & Ahmed, R. A. (2020). Advanced closed-loop communication training: the blindfolded resuscitation. BMJ Simulation and Technology Enhanced Learning, 6, 235-238.
Müller, M., Jürgens, J., Redaèlli, M., Klingberg, K., Hautz, W. E., & Stock, S. (2018). Impact of the communicaiton and patient hand-off tool SBAR on patient safety: a systematic review. BMJ Open, 8, e022202. doi:doi:10.1136/bmjopen-2018-022202
Sarfati, L., Ranchon, F., Vnatard, N., Schwiertz, V., Larbre, V., Parat, S., . . . Rioufol, C. (2019). Human‐simulation‐based learning to prevent medication error: A systematic review. Journal of Evaluation in Clinical Practice, 25, 11-20. Retrieved from https://doi.org/10.1111/jep.12883